Periacetabular Osteotomy
Introduction
Periacetabular osteotomy (PAO) is a surgical treatment for hip dysplasia which preserves and improves the function of the patient’s own hip joint rather than replacing it with an artificial one. The goal of the PAO is to surgically reposition the acetabulum (socket) to adequately cover the femoral head (ball) in order to reduce or eliminate pain, restore function, and maximise the functional life of the dysplastic hip.
PAO was initially developed by Professor Ganz in Bern, Switzerland, and is therefore often known as the Bernese PAO or the Ganz Osteotomy. PAO is designed to correct the major mechanical problems in acetabular dysplasia, which include excessive pressure of the femoral head on the rim of the acetabulum and instability of the femoral head within the acetabulum. Dr. Boyle regularly performs PAO surgery for patients from throughout New Zealand, undertaking approximately 50 PAOs per year, and is the highest volume PAO surgeon in New Zealand.
Surgical Summary
The ideal PAO patient has minimal damage to the articular cartilage inside the hip joint. In general, such patients have little or no narrowing of the cartilage space on regular x-rays and can flex their hips to at least 90° with minimal pain.
PAO is performed by Dr. Boyle through a minimally-invasive technique, using a single 8-10 cm oblique incision at the front of the hip, often called a "bikini" incision, that blends nicely with the natural skin crease of the hip.
Typical minimally-invasive PAO scar (one year following surgery).
Minimally-invasive PAO scars typically fade with time. The image above was taken one year after right PAO and two years after left PAO.
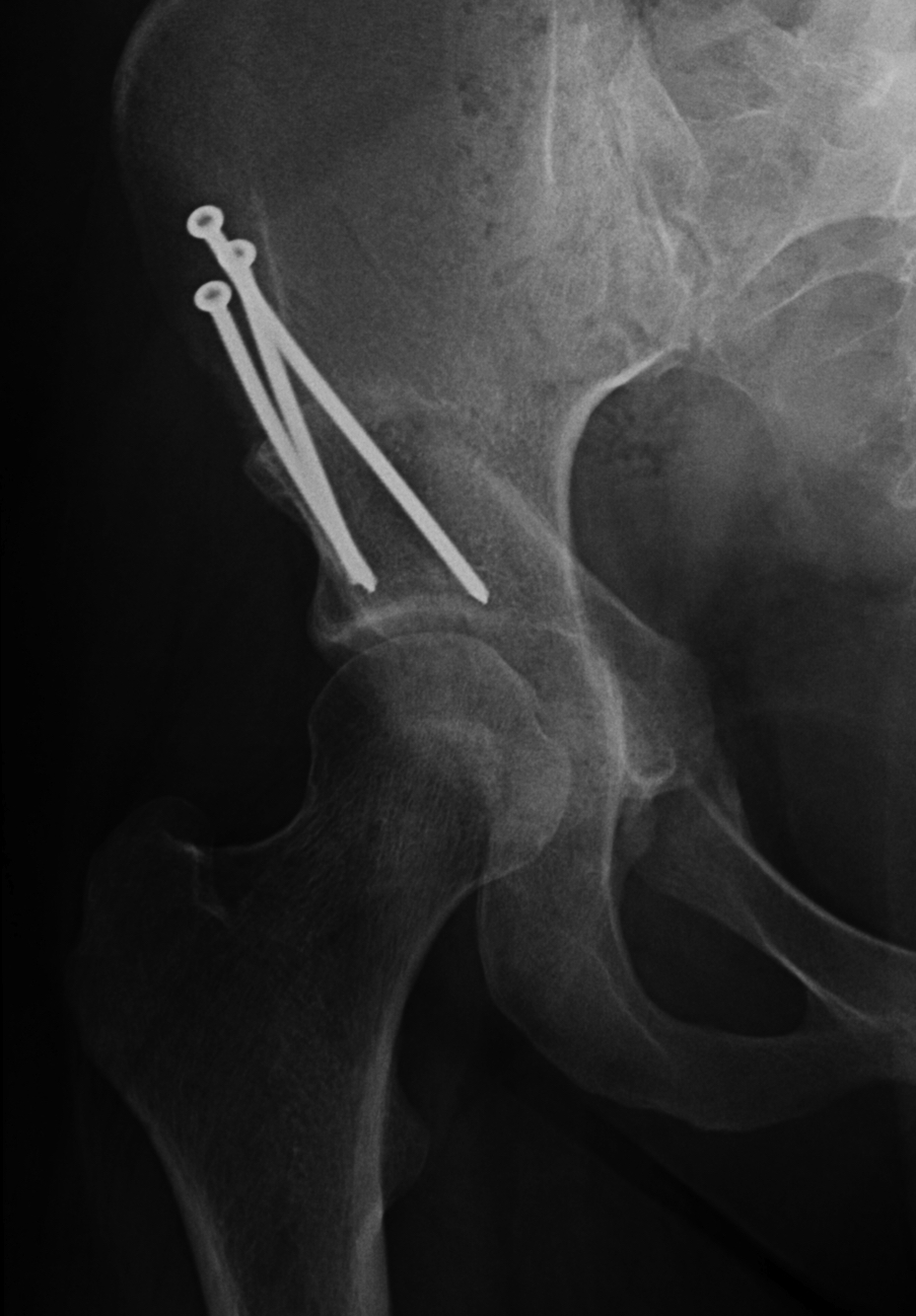
Dr. Boyle cuts the bone around the acetabulum and then rotates the acetabulum into a more stable, horizontal position of coverage over the femoral head. The pressure from the femoral head is thus transferred to the central portion of the acetabulum, where the articular cartilage is designed to accept this pressure. Three to four small screws are used to hold the bone in place while it heals.
Before PAO
After PAO
Additional hip procedures are sometimes required at the same time as the periacetabular osteotomy, such as arthroscopy (“key-hole” hip surgery to inspect and manage labral or cartilage tears), arthrotomy (opening the hip joint through the same incision as the PAO to repair joint damage), osteoplasty (shaving prominent bone that may cause impingement after PAO), and proximal femoral osteotomy (cutting and realigning the head and upper end of the femur). Between six and twelve months after PAO surgery, most patients undergo screw removal as a brief outpatient procedure.
Outcomes
After the PAO has healed with return of hip motion and strength, Dr. Boyle encourages the highest level of reasonable activity that the hip joint will allow. A corrected dysplastic acetabulum is still at risk for damage by overuse. Although most PAO patients are able to jog and some even run marathons without a problem, the long-term impact on their joints is not yet known. In general, since dislocation is not a risk after PAO, there are no positional restrictions as there can be after total hip replacement.
Dr. Boyle and his international hip preservation colleagues consider failure of PAO to mean lack of improvement in hip pain, or an increase in hip joint stiffness serious enough to limit patient activities. In such situations, a joint-replacing procedure of some type may become necessary.
Dr. Boyle has undertaken extensive training in PAO surgery at Boston Children’s Hospital (BCH), one of the highest-volume PAO hospitals in the world. Of the more than 2000 patients who have undergone PAO surgery over the last 20 years at BCH, only around 40 have required a Total Hip Replacement (THR). The patients who have required THR have been the ones who had the most damaged cartilage before their PAO surgery.
Ten years after their PAO, more than 90% of patients have little or no pain and well-functioning hips; at twenty years after their PAO, approximately 70% of patients still have little or no pain and well-functioning hips; at thirty years after their PAO, approximately 35% of patients sill have little or no pain and well-functioning hips. In appropriate patients who, along with their surgeon, select PAO as the treatment of choice, hip pain and function is expected to be greatly improved by the surgery for a minimum of ten years and, hopefully, for a lifetime.